Introduction
Tafasitamab (MOR208) is an Fc-enhanced, humanized, monoclonal antibody that targets CD19 and has shown promising clinical activity in patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL). CD19 is homogeneously expressed among different B-cell malignancies, and the binding of tafasitamab to CD19 directly mediates cell death, induces antibody-dependent cellular cytotoxicity and antibody-dependent cellular phagocytosis.
Aiming to potentiate the tafasitamab-mediated "eat me" signal, we tested a combination with a CD47-directed monoclonal antibody (mAb) to inhibit the CD47/SIRPα "don't eat me" signal and further enhance macrophage-mediated phagocytosis. Preclinical studies demonstrated that blocking the CD47/SIRPα checkpoint in combination with antibodies, such as rituximab, increased phagocytosis by macrophages, resulting in effective anti-tumor effects in non-Hodgkin lymphoma (NHL) (Chao, et al. 2010). Additionally, the combination of the anti-CD47, magrolimab, and the anti-CD20, rituximab, demonstrated beneficial outcomes for patients with refractory NHL (Advani, et al. 2019).
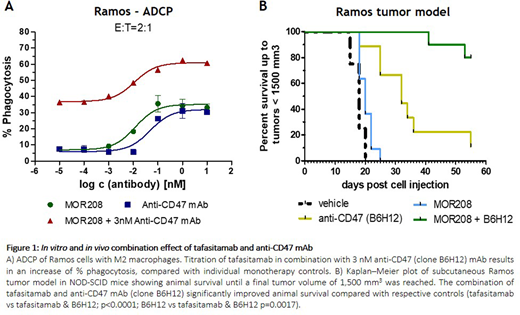
Here, we present in vitro and in vivo data on the combinatory effect of tafasitamab and an anti-CD47 mAb in preclinical models of Burkitt's lymphoma (BL).
Methods
During in vitro studies, CD14+ monocytes were isolated from the whole blood of healthy volunteers and differentiated with 50 ng/mL M-CSF for 6 days. ADCP was analyzed by flow cytometry in co-culture experiments with Ramos cells (BL) after 3 hours of treatment with tafasitamab and anti-CD47 mAb (clone B6H12).
In vivo, the combination of tafasitamab with an anti-CD47 mAb was tested in a Ramos disseminated survival and subcutaneous tumor model in SCID and NOD-SCID mice, respectively. In both models, tafasitamab was administered therapeutically twice a week either at 3 mg/kg (disseminated) or 10 mg/kg (subcutaneous) for max. 4 weeks. The anti-CD47 mAb was administered at 4 mg/kg three times per week. Main study readouts were to assess animal survival and any delays in tumor growth.
Results
The combination of tafasitamab + CD47/SIRPα checkpoint blockade enhanced ADCP activity of primary M2 macrophages on BL-derived Ramos cells, in comparison with the anti-CD47 mAb or tafasitamab monotherapies (Figure 1A). In vivo, a significant increase in anti-tumor activity was observed with the combination of tafasitamab + anti-CD47 mAb. In the Ramos disseminated survival model, the combination showed an increased life span (ILS) of >182% compared with tafasitamab monotherapy control, with an overall survival of all animals treated with the combination (15/15) until the end of the study (Day 99 post-cell injection).
Additionally, pronounced anti-tumor efficacies were detected in the Ramos subcutaneous tumor model. Here, the combination resulted in a significant delay in tumor growth compared with the tafasitamab or anti-CD47 mAb monotherapies (ILS >175% tafasitamab and ILS >72% anti-CD47 mAb vs tafasitamab + B6H12) (Figure 1B).
Conclusions
The ADCP activity of primary macrophages was increased by combining tafasitamab with an anti-CD47 mAb in vitro, resulting in enhanced anti-tumor activity compared with tafasitamab or anti-CD47 mAb monotherapies in vivo. Overall, results indicate the combination of tafasitamab with a CD47/SIRPα checkpoint blockade may be a promising novel combination approach for lymphoma therapy.
Mangelberger:MorphoSys AG: Current Employment. Augsberger:MorphoSys AG: Current Employment. Landgraf:MorphoSys AG: Current Employment. Heitmüller:MorphoSys AG: Current Employment. Steidl:MorphoSys AG: Current Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal